NUB application
Assessment
NUB inquiry procedure
Assignment of status by the Institute for the Hospital Remuneration System (InEK)
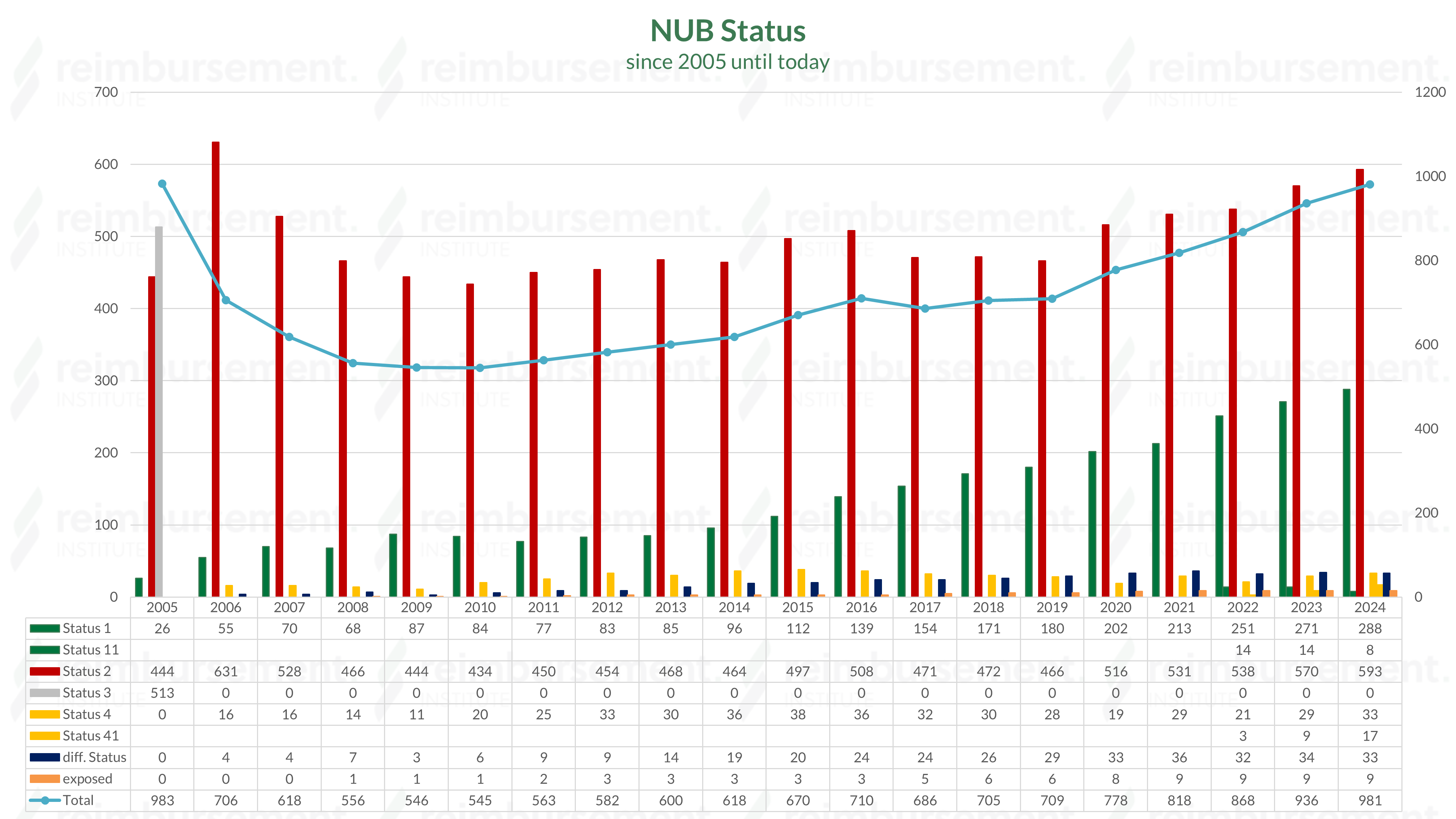
The evaluation of the submitted NUB requests (colloquially NUB applications) is carried out by the InEK by the end of the year and provided with a status. These are published in January of the following year.
The following status can be assigned to requests received on time:
Status 11
Criteria of the NUB agreement of the contracting parties are fulfilled as of the date of approval.
Plain text: Appropriate remuneration of the requested method via DRG or ZE could not be determined > The hospital can enter into negotiations with the payers from the time of approval.
Status 2
Criteria of the NUB agreement of the contracting parties are not fulfilled.
Plain text: Appropriate remuneration of the requested method via DRG or ZE could be determined or other reasons > The hospital cannot enter into negotiations with the payers.
Status 3
Not fully processed within the set deadline.
Plain text: The InEK was unable to process the request within the specified timeframe and consequently could not evaluate it > The hospital cannot enter into negotiations with the payers.
Status 4
Criteria of the NUB agreement for assessment not sufficiently presented.
Plain text: The InEK was unable to make a conclusive statement > In justified individual cases, it is possible for the hospital to negotiate a reimbursement with the payers.
Status 41
Criteria of the NUB agreement for assessment not sufficiently presented.
Plain text: The InEK was unable to make a conclusive statement > In justified individual cases, it is possible for the hospital to negotiate a reimbursement level with the payer from the time of approval.
What follows after the NUB inquiry process?
If a new examination and treatment method has been assigned a negotiable status, this will generally remain in place until it is integrated. As a rule, integration into the standard care system via DRGs or procedures is carried out after three years, if sufficient data material has been collected for the calculation. This process can be shortened by the provision of supplementary data, which the calculation hospitals can submit upon separate request by the InEK.
NUB fee negotiation
Submitting hospitals must negotiate the so-called NUB fees for innovative pharmaceuticals, medical devices and procedures annually, insofar as the request has been assessed by the InEK with a corresponding status. This can be done as part of the annual budget negotiation, but also in an isolated NUB negotiation, e.g., right at the beginning of the year. NUB fees are extrabudgetary and represent the possibility of additional, so-called extrabudgetary revenues for hospitals. In principle, NUBs are subject to the efficiency requirement.
Additional costs can be negotiated if they have a verifiable added value based on standard care that justifies the resulting increased procedural costs.
Note: A negotiable assessment of the new examination and treatment method does not automatically lead to a successful negotiation between the service provider and the payer (health insurer).
Integration into standard care
In most cases, reimbursement is made via a fee per case (DRG). Reimbursement via the G-DRG can take place in various ways.
- Based on the data, the costs of the new procedure could be included in the DRG system. Reimbursement is made via the adjusted relative weight of a DRG.
- The OPS code documenting the procedure / medication is used as a trigger and is (co-)responsible for the DRG allocation alone or in combination with other codes or characteristics.
- There is a redesign / differentiation of existing base DRG groups.
- Remuneration via an additional fee is created in order to maintain the homogeneity of the DRGs.
NUB Judgment from 05.12.2019
Quintessence: NUBs that have been given a negotiable status by the InEK, have been used by the requesting hospital, and have consequently incurred costs, must be compensated by the payers. This applies to the period from the publication of the NUB status (usually at the end of January of each year and retroactively as of January 1) until the time of the NUB budget negotiation. A plausible and complete documentation on the part of the hospitals regarding the reason for the use of the NUB is obligatory!
more on this topic plus free download of the whitepaper